WHAT IS COVID19 FOR ME- AN ANECDOTE
COVID-19 has created tremendous pressure on the whole world and ruined the world’s economy, putting people in lockdown with social restrictions like caged animals. However, for medical professionals, especially nurses, it’s a war with an invisible enemy putting our lives at risk.
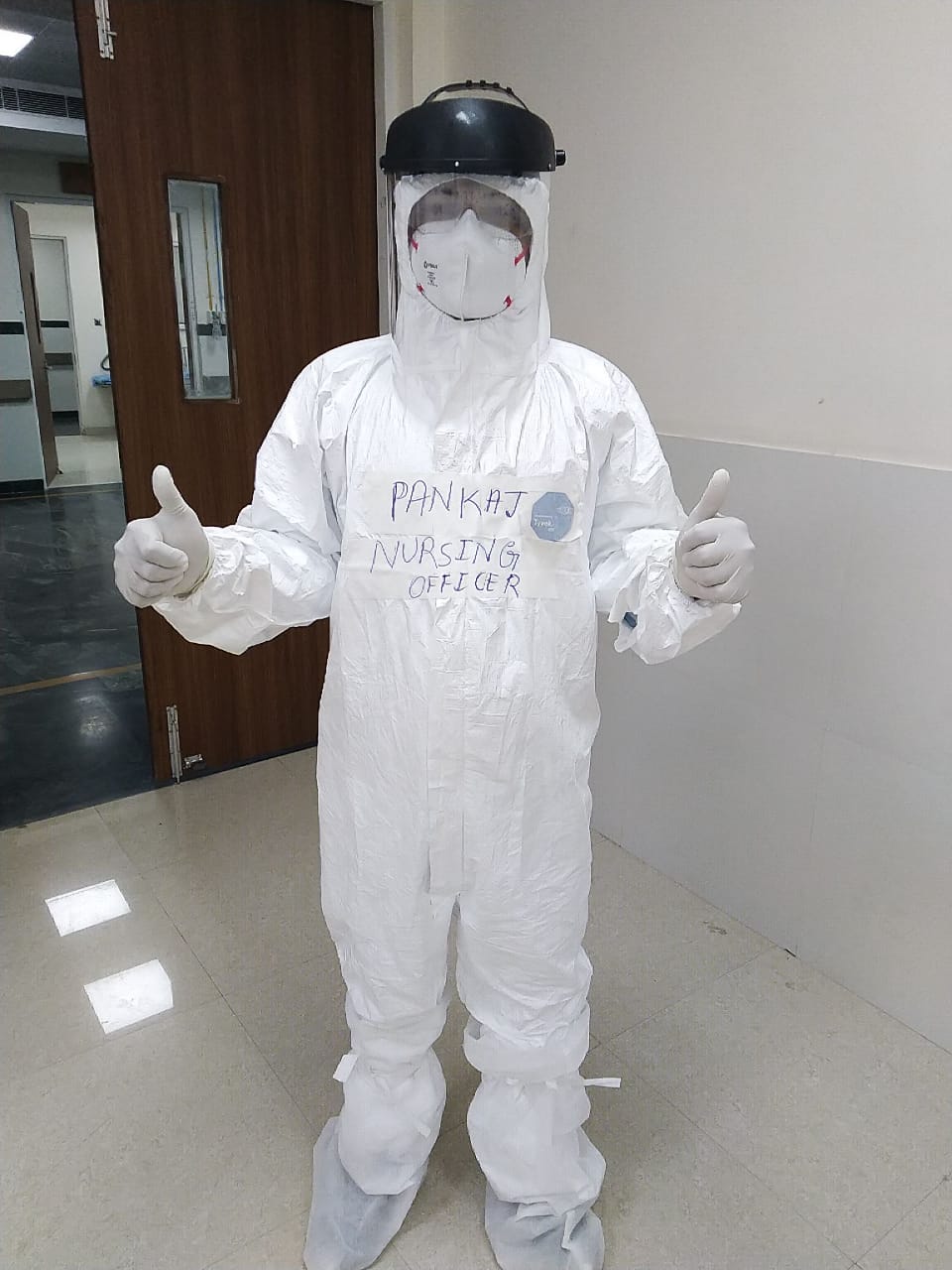
First day of being in the COVID-19 unit
Due to the peak wave of covid19 pandemic throughout the United Kingdom (UK) in June, priorities have changed from elective surgeries to managing this pandemic. I am bound to work in the COVID unit other than my routine ward, i.e. Elective unit. It has created unimaginable anxiety, frustration and even panic behaviour; I felt nervous and frightened; What the hell is this? What if happen if it comes? How I can put myself at risk as the media almost killed my esteem with the continuous feeding of pessimistic news? I made my decision the best way to cope with something is to face it; it is not me whole medical fraternity is in a war zone has smoothened my mind
How did we work?
It’s a ward with 15 isolation beds especially redesigned for COVID-19. Infection control measures are our nursing team’s main task as we must protect and accommodate all COVID-19-positive cases who need symptomatic treatment, wherein all critical cases are in Intensive care units. Initially, I was trained to wear FF3 masks after completing the “fit to wear” test. As a team, all follow the government’s infection guidelines based on scientific evidence. Protocols are changing daily, so we all must mend ourselves to changes happening. Each team member, from doctors to health care assistants and support staff, followed standard guidelines for handwashing, cleansing equipment, wearing masks and gowns and their safe disposal. Everything that comes in contact with the patient is treated as orange waste. The most admirable thing was our assertiveness when someone didn’t follow the standard precautions. Concerning PPEs, we use a Disposable FF3 mask, plastic apron and visor for patients with active symptoms, whereas asymptomatic cases are treated with normal surgical masks, visors and aprons. We have relied more on safe staffing, limited exposure and frequent hand washing. So more than 2 months in the COVID ward with almost 10 to 12 staff to look after 15 patients, we managed to treat approximately 150 to 200 patients by protecting ourselves.
How are we supported in diagnosis and treatment?
Travel history, COVID swabs, sputum culture, and blood for C-reactive protein, White Blood Cells, lactate, and finally, Chest X-ray for nasty chest there is a continuum of tests for confirmative diagnosis. Precision and accuracy of swabs is vital in early diagnosis and prompt treatment. All nursing staff and health care assistants are trained to take appropriate swabs. The protocol is to take a swab on admission, 2 nd swab after 48 hours if it comes back negative, and 3 rd swab on 7 th day. (Swab testing protocols do change as per new pieces of evidence) It’s very hard to take the swab as it literally tears patients’ eyes. Many were reluctant to take swabs; it’s our patience and dedication to console their swabs. Sometimes, it’s hard to diagnose as many tests come negative despite all active symptoms. Poor prognosis for the elderly with comorbidities has finally put them on End of life care. It is very annoying as hospitals manage their last rituals instead of families. Conversely, overwhelming greeting cards, social media, personal wishes, and extended moral support from management and the public for those who recovered have satisfied our work.
What did we learn?
As the cases stabilised over the months, management finally decided to change the COVID unit into the surgical unit as they have a separate unit for all suspected COVID patients. Things to take away from us are that teamwork, assertive communication, autonomy, continuous support from management, well-being support for those involved in treating COVID-19, resilience and nursing leadership can ease the burden of those who handle a pandemic like COVID-19. However, we are treating whoever is admitted to the hospital as COVID-positive. I feel covid19 experience has boosted my resilience.
Note: It’s all my personal experience of being in the COVID unit; however, it may contradict the views of others






I gotta say, it’s an eye-opening account of a nurse’s life in a COVID-19 unit. It’s really fascinating to see how you dealt with all those emotions and challenges on the frontline. I admire the way you highlight the importance of teamwork, communication, and resilience during such tough times. It’d be cool to read more about the bigger picture, like how the pandemic affected healthcare workers’ mental health, burnout, and the long-term impact on the healthcare system. Also, it’d be great to hear about other healthcare workers’ experiences to get a fuller picture of what everyone went through during this crazy time. Keep up the great work!